What to know about HIV false-positives ?
A
false-positive HIV test occurs when a test incorrectly indicates that a person
has contracted the
virus. Receiving a false positive can inspire conflicting
feelings. People may wonder what they can
or should do next.
In this
article, we suggest some next steps for people who have had
false-positive HIV test results. We also provide detailed information
about the HIV testing process.
A person knows
that they have had a false positive when an initial test indicated that they
had HIV but a follow-up test was negative.
A false
positive typically results from the test incorrectly identifying non-HIV
antibodies as HIV antibodies.
What to
do after a false-positive result
After
receiving the initial result, the healthcare provider will perform an
additional test to ensure that the result is accurate.
If the
second result is also positive, it confirms the presence of HIV.
In this
case, a healthcare provider will provide support and information about
treatment options.
If the
follow-up test is negative, it means that the first test was incorrect.
Below are
some tips that can help a person deal with a false-positive result.
Seek
support
When a
person learns that they may have a chronic condition, it can be stressful or
overwhelming, even while waiting to receive the results of the second test.
If the
second test returns a negative result, a person may experience conflicting
emotions. It can be helpful to seek support during this time, from family,
friends, or a partner.
Some
people may wish to discuss their emotions with a mental health professional,
such as a therapist.
Find the
reason for the result
It is
important to discuss the cause of a false-positive result with the doctor.
Some
false positives stem from technical mix-ups, incorrect labeling, or a person
misreading the result.
There can
also be medical mechanisms behind false positives.
For
example, a false-positive reading may indicate that the person has an
autoimmune disorder or another underlying medical condition. In this case, it
may be a good idea to investigate further.
Consider
repeating the test in a few months
If a
person receives a negative follow-up result but thinks that they may have been
exposed to the virus in recent weeks, it is important to take another test in
2–3 months.
This is
because it takes several weeks for HIV antibodies to reach detectable levels in
the bloodstream.
Doctors
call the time in which levels of antibodies are undetectable the "window period." HIV test results are often
negative during this period, though the person has contracted the virus.
Take
steps to prevent HIV
Everyone
should take precautions to avoid contracting or transmitting the HIV virus. To
do this:
·
Use
condoms during all sexual activity.
·
Consider
limiting the number of sexual partners.
·
Refrain
from using oil-based lubricants with condoms.
·
Do not
share needles if using intravenous drugs.
·
Consider
male circumcision.
According
to the World Health Organization (WHO), medical male circumcision may reduce
the risk of heterosexually acquired HIV by 60 percent.
Some
people have a higher risk of contracting HIV, including people whose sexual
partner or partners have the virus. In this case, taking pre-exposure
prophylaxis, or PrEP, therapy can reduce the risk of contracting it.
People
who may have been exposed to HIV can take post-exposure prophylaxis, or PEP,
medication within 72 hours. This may prevent them from contracting the virus.
HIV
testing
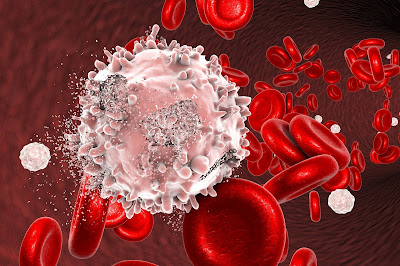
Healthcare
providers usually test for HIV with an immunoassay. This detects HIV antibodies
and proteins in the bloodstream.
The
immunoassay requires a blood sample. Results may be available in minutes, or
they can take up to a week, depending on the type of blood sample.
Due to
the risk of inaccurate results, healthcare providers repeat the test to confirm
the initial finding, according to WHO best
practices. They may use the original blood sample or a new one.
People
with a high risk may undergo a different type of HIV test called a nucleic acid
test, or a NAAT. These are expensive and so are not routinely used for HIV
diagnosis.
Inaccurate
results
False-positive
results are uncommon, according to the Centers for Disease Control and Prevention (CDC).
The CDC
also estimate that the specificity, or accuracy, of testing is 99.6 percent.
The other
type of inaccurate result is a false negative. It occurs when an initial result
is negative, but subsequent testing indicates that the person does have the
virus.
False
negatives usually occur in the early stages of HIV, before detectable levels of
antibodies build up in the bloodstream.
Who
should get tested for HIV?
The
CDC recommend that
everyone ages 13–64 get tested for HIV at least once. Those at high risk should
undergo annual testing.
Men who
have sex with other men may wish to consider getting tested more frequently,
possibly every 3–6 months.
Factors
that increase a person's risk of contracting HIV include:
·
having
sex not protected by condoms
·
sharing
needles and other drug equipment
·
having
sex with a person who has HIV or is at high risk of HIV
·
having
another sexually transmitted infection
·
being an
uncircumcised male
Pregnant
women should undergo HIV testing so that they can receive treatment if the
results are positive. Receiving treatment during pregnancy reduces the risk of
transmitting HIV to the baby.
Takeaway
A
false-positive HIV test result can cause conflicting emotions. It is important
to discuss the reasons for the inaccuracy with the healthcare provider and ask
about options.
Everyone
should receive HIV testing at least once. Pregnant people and those with
increased risk should undergo testing more often.
For
people in the United States, this CDC locator can help identify nearby HIV
testing.
To
prevent the virus' transmission, use a condom during sexual activity, refrain
from sharing needles, and consider male circumcision



Dr. Imoloa has really made me so much believe in him by getting me cured with his herbal treatment. i really appreciate you Dr.imoloa for bringing back happiness to my life again. thank you so much,friends join me to thank him for what he has actually done for me i pray to you all for a good life and good health, and most especially to you Dr. imoloa Thanks
ReplyDeleteI have been suffering from (HERPES SIMPLEX VIRUS) disease for the past four years and had constant pain, especially in my knees. During the first year,I had faith in God that i would be healed someday.This disease started circulating all over my body and i have been taking treatment from my doctors, few months ago i came on search on the internet if i could get any information concerning the cure of this disease, on my search i saw a testimony of someone who has been healed from (HERPES SIMPLEX VIRUS) by this Man Dr imoloa and she drop the email address of this man and advise we should contact him for any sickness that he would be of help, so i wrote to Dr. imoloa telling him about my (HERPES Virus) well after all the procedures and remedy given to me by this man few weeks later i started experiencing changes all over me. I am now here to testify that i am no longer a herpes patient, I have experience a total transformation in my life,for all herpes patients get your herbal medicine to cure your sickness. And there has being rapid improvement in my health, I no longer feel pains and I wake up each morning feeling revived. So friends my advise is if you have such sickness or any other at all,you can contact him on drimolaherbalmademedicine@gmail.com, you can still reach him on whatssap- +2347081986098
CANCER
EPILEPSY.
GENPILENCIN.
HIV AIDS.
DIABETICS
STROKE.
BREAST ENLARGEMENT...PENIS ENLARGEMENT, H.P.V TYPE 1 TYPE 2 TYPE 3 AND TYPE 4. TYPE HUMAN PAPAILOMA VIRUS HERPES. SYPHILIS. HEPATITIS A B and C.